Obturator to Femoral Nerve Transfer for Femoral Nerve Palsy Using a Modified Technique-Juniper-Publisher
Juniper Online Journal of Orthopedic & Orthoplastic Surgery
Introduction
Though uncommon, femoral nerve palsies are
potentially devastating injuries which can occur as a result of
penetrating trauma or malignancies, however the most common cause is
inadvertent iatrogenic injury following intra abdominal surgery such as
gynaecological/vascular surgery or total hip replacement [1].
We present a case of iatrogenic femoral nerve injury with a delayed
presentation resulting in an 8.5cm nerve defect, which was managed with
both traditional cable grafting and a contemporary nerve transfer
utilising a modification of an existing technique.
Case Report
In September 2015 a 49 year old female presented to
our institution 6 months following a laparoscopic inguinal hernia repair
which had resulted in a complete transection of the right femoral
nerve. There was a 6 month delay in diagnosis of the iatrogenic injury.
The patient had an extraperitoneal exploration of the right groin which
confirmed the diagnosis, and an 8.5cm nerve defect at the level of the
inguinal ligament was cable grafted with 4 cables sural nerve grafts.
After discussion with the patient and appropriate review of the
literature and cadaver dissection, the patient had a nerve transfer
procedure 3 weeks following the cable grafting.
Procedure 1
In conjunction with General Surgical colleagues a
supra- inguinal extraperitoneal approach was performed exposing the
femoral neurovascular bundle in the right iliac fossa. This incision was
then extended distally and the inguinal ligament was divided and later
repaired for exposure of the nerve. A prominent neuroma was identified
where the nerve was divided, associated with mesh and metallic tacs from
the hernia. Ipsilateral sural nerve was harvested and a reversed cable
graft using four 8.5cm cables was used to close the defect.
Procedure 2
Nineteen days after the first operation an obturator
to femoral nerve transfer was performed. An anterior longitudinal
incision incorporating the existing scar was used to expose the distal
end of the cable graft, the distal femoral nerve and its terminal
branches. The medial sensory branch and the branches to the rectus
femoris and vastus lateralis were identified and the latter two
confirmed to be non functional with electrical stimulation. The anterior
branch of the obturator nerve was identified and traced distally to
identify the branch entering gracilis. The nerve to gracilis was
transected distally and passed over the adductor longus muscle to reach
the femoral nerve. It was then redirected sub muscularly under the
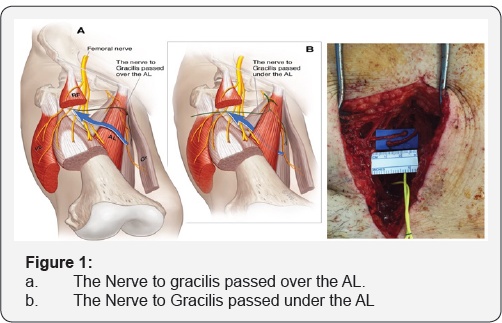
adductor longus muscle (Figure 1).
With this more direct route, the end of the gracilis branch was able to
reach four centimetres more distally. The nerve to gracilis was then
neurotised to the femoral nerve branch to rectus femoris. The
neurotisation was undertaken under microscope magnification with 9-0
S&T sutures (Insert Trade Details) and reinforced with Tiseel™
fibrin glue (Baxter pharmaceuticals).
Discussion
Complete femoral nerve injuries are uncommon and
usually leave the patient with significant morbidity, requiring orthoses
for simple mobility. Traditionally a nerve defect of this size would be
managed with autologous cable grafting as initially performed. The
large size of the nerve defect and also the significant distance from
the distal end of the graft to the neuromuscular junction result in a
poor prognosis for functional recovery. Whilst tendon transfers provide a
good reconstructive option for some neurological injuries, (example
radial nerve palsy), there are few satisfactory options available for
femoral nerve palsy. Fischer et al. [2]
reported on a hamstring transfer after soft tissue sarcoma resection
with significant complications and modest results of extension force.
Nerve transfers have been well described in the literature for upper limb reconstruction [3].
There is in contrast a paucity of reconstruction options in lower limb
nerve injury. Nerve transfers provide an attractive option, as
performing the neurotisation distally minimises the distance and hence
time required for neural regeneration and ultimately functional
recovery. Motor end plates are known to undergo extensive change post
denervation and functional reinnervation is unlikely beyond 18 months
due to progressive fibrosis [4].
This case also posed further time pressure as referral to our
institution was delayed by 6 months since the nerve injury. By
performing the second procedure of the obturator to femoral transfer,
viable axons were delivered approximately 13cm closer to the
neuromuscular junctions providing greater potential for reinnervation
prior to loss of the motor end plates.
The pattern of the femoral nerve branching pattern has been previously described in a cadaver dissection by Tung et al. [3]. There have only been two previous papers in the literature discussing case reports of 3 similar procedures. Campbell et al. [5]
reported a single case of total obturator to femoral nerve transfer 3
months post schwannoma resection with good functional result. This was
performed above the inguinal ligament. Goubier et al. [6]
conducted a cadaveric feasibility study in 2012 confirming the
possibility of performing a subcutaneous transfer of two obturator motor
branches to the femoral nerve in the thigh.
Tung et al. [3]
reported on 2 cases of a subcutaneous obturator to femoral nerve
transfer for complete femoral nerve injury- 1 performed acutely and the
other 5 months post injury. The second patient was also supplemented
with a superior gluteal nerve transfer after the first patient had
incomplete recovery and an inability to climb stairs. This showed
encouraging results. In our patient we have combined the existing
obturator to femoral nerve transfer and added a cable graft in an
attempt to provide a belt and braces reconstruction. We also determined
that directing the gracilis branch deep to adductor longus rather than
superficial to this muscle provides an increase in effective length of
the nerve, allowing a more distal nerve repair, which is theoretically
beneficial.
Iorio et al. [7]
noted the proximity and potential of the anterior branch of the
obturator nerve to gracilis in femoral nerve injuries. In their
cadaveric study they proposed using this nerve for a donor for cable
grafting, hypothesising that a motor nerve may maximise functional
outcomes. They also noted that the average donor length was 11.4cm. The
anterior branch of the obturator nerve has also been considered for
restoring other neurological losses. In a cadaveric study in 2014,
Houdek et al. [8]
deemed it feasible to transfer the anterior branch of the obturator
nerve to pelvic nerves in order to restore bowel and bladder function.
Interestingly Spiliopoulos et al. [9]
published a case report of the reverse nerve transfer - femoral branch
to obturator to restore adduction following another iatrogenic injury.
They reported a good outcome with full power and normal gait.
Conclusion
We present a novel 'belt and braces' approach for
managing this unusual injury, using a modification of a nerve transfer
which has only been reported in the literature three times previously to
our knowledge.
To read more articles in Journal of
Orthopedic & Orthoplastic Surgery
To
Know More about Juniper Publishers click
on: https://juniperpublishers.com/




Comments
Post a Comment