Breast Reconstruction Using a Latissimus Dorsi Flap with Skin Graft after Total Paliative Mastectomy in a Large Advanced Carcinoma Breast-Juniper-Publisher
Juniper Online Journal of Orthopedic & Orthoplastic Surgery
Case Presentation
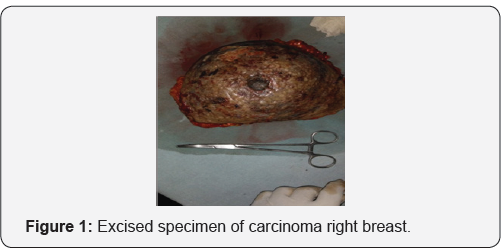
A 50-year-old female diagnosed an advanced carcinoma
of the right breast. After four cycles of neoadjuvent therapy, tumour
size was decreased but still it was 15* 10 cm in dimension, free from
chest wall, multiple ulcerations with foul smelling discharge with liver
metastasis. Patient underwent a right sided total paliative mastectomy
and immediate breast reconstruction with a right sided latissimus dorsi
(LD) myocutaneous flap, but the defect was very large, flap and skin was
opposed under tension. On seventh post operative day, it was noticed
that upper flap was not apposed, there after patient was subjected for
skin graft. Post operative period was uneventfull. Patient is sent into
radiotherapy department for further managment.
Discussion
The latissimus dorsi (LD) flap was first described in the seventies for breast reconstruction [1].
Early attempts to increase the volume of the flap by including fascial
extensions were described by Hokin in 1983 and then by Hokin and
Sliverskiold in 1987 taking the whole muscle and lumbar fascia with the
largest possible skin paddle running obliquely along the back. The skin
paddle could be partly or wholly de-epithelialized for added volume [2,3].
In the current study, we have designed the skin paddle in a transverse
direction and we were still able to harvest enough fat from the scapular
and lumbar regions. The transverse scar was quite acceptable to
patients (Figure 1).
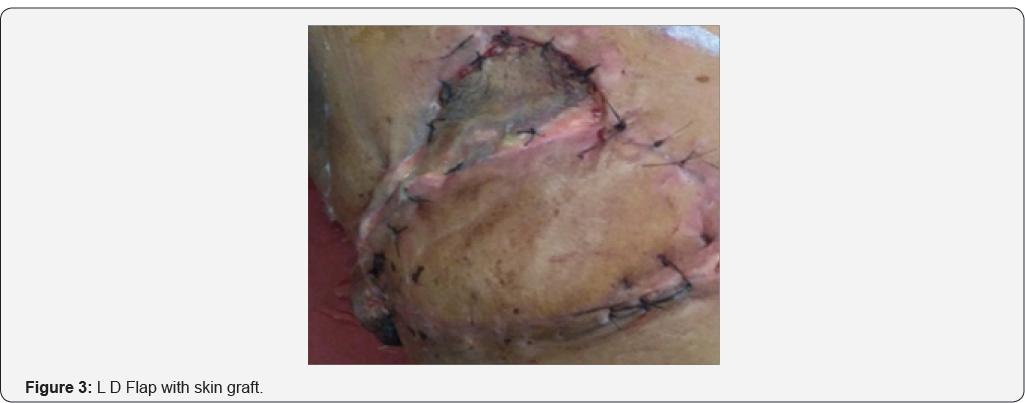
Some authors have abandoned the use of the
fleur-de-lis skin paddle design because of the resulting extensive
donor-site scar and have adopted to use the transverse skin paddle
instead, where it can be hidden in the bra line [4]. Nevertheless, dorsal flap necorsis is a potential problem and it has been variably reported
by several authors. Chang et al. [4] reported 16% necrosis rates in 75 patients while Delay et al. reported 3% incidence in 100 patients [4]. In this case report patient developed necrosis of the edges of the flaps. It required reoperationwith skin graft (Figure 2). It is important that the primary wound closure of the donor site should be relatively tension-free [4].
Inadvertently excessive thinning of back flaps as well as greater
tension created in wound closure due to poor skin paddle design have
resulted in necrosis and wound breakdown (Figure 3)
. On the other hand, the LD flap itself is a very reliable flap with
very low incidence of partial or complete necrosis. It is noteworthy
that a higher incidence of fat necrosis is expected in larger flaps due
to the harvest of some fat from beyond the borders of the muscle with
its random blood supply [4].

Conclusion
The LD flap is a good alternative that can be offered
for autologous breast reconstruction in a laregr breast cancer patient
were palliation is required. The flap is primarily indicated for those
who are not suitable candidates for TRAM flaps or for that group of
patients who would prefer the back donor site and are reluctant to
proceed for the prolonged recovery of the pedicled TRAM or for the
possible morbidity and the complexity of free tissue transfers. The
disadvantages of the flap lie in the high incidence of seroma , mild
contour deficiency of the back, limitations in the size of the flap
making it unsuitable for certain groups of patients who have very large
and/or severely ptotic breasts which is managed ia=n association with
split skin graft.
To read more articles in Journal of
Orthopedic & Orthoplastic Surgery
To
Know More about Juniper Publishers click
on: https://juniperpublishers.com/



Comments
Post a Comment