Microsurgical Reconstruction with Free Osteocutaneous Fibular Flap for Mandibular Osteoradionecrosis with Pathological Fracture: A Case Report-Juniper-Publishers
Juniper Online Journal of Orthopedic & Orthoplastic Surgery
Introduction
Osteoradionecrosis is the long term and most serious
side of radiotherapy. The definition of osteoradionecrosis is generally
accepted as presence of exposed bone in an irradiated field, which fails
which to heal within a three-month a period [1].
Treatment of osteoradionecrosis is a challenging problem. There is a
variety of treatment options and no universal approach to management, as
this depends on institutional or individual experiences. Early case of
osteoradionecrosis treated with hyper baric oxygen therapy, antibiotics,
tocopherol and pentaxyphyllin [2].
Conservative debridement may be necessary to remove spicules of
devitalised bone particularly if the adjacent tongue is abraded.
Patients who have osteoradionecrosis are traditionally treated with HBO
alone or combined with debridement. Segmental mandibulectomy and
reconstruction are necessary in patient with severe osteoradionecrosis
who do not improve with conservative treatment [3,4].
Case Report
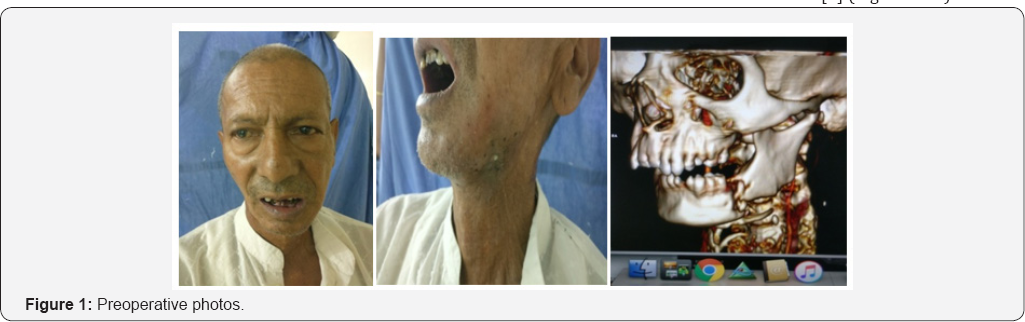
We report a case of 72 year old male patient with
pathological fracture with draining cutaneous sinus. Patient had
diagnosed with hypo- pharyngeal carcinoma 10 year back. Patient had
received radiotherapy and chemotherapy immediately after diagnosis.
Patient was complaining of difficult and pain while opening of mouth 6
month back. Patients had developed swelling at lower border of mandible
which after few days ruptures with pus discharge. Patients had no
history of trauma to face, dental extraction, or any oral surgery. On
clinical examination patient had scared and lusterless oral mucosa.
There was a draining sinus over owner border of cheek. Mandibular
crepitus with severe tenderness was present. Patient was first evaluated
for any possible recurrence. Ct scan was done to know about site of
fracture and extent of osteomyelitis. PET CT scan and Biopsy was done to
rule out malignancy or recurrence.
Pus culture was done suggestive of streptococcal
infection sensitive to ampicillin Antibiotic started 1 week before
actual procedure. Patient was posted for operation after obtaining
physical fitness. Under general anaesthesia lip splitting incision was
taken. Wide local excision of draining sinus with fibrosed soft tissue
and segmental mandibulectomy was done to obtain healthy bleeding edges
of bone and skin. Recipient vessel explored. Facial artery was
thrombosed till its origin. External carotid artery was prepared as
recipient artery and common facial and external jugular vein was
prepared as recipient vein. Measurement of defect of skin and bone done
and template
prepared. Free osteocutaneous free fibula flap harvested under
tourniquet control. Adequate vessel and bony preparation were done. Bony
fixation was done with titanium plate and screw. Partial inset was
given. Arterial and venous anastomoses were done with external carotid
artery and common facial vein. Oral cavity closed in layer. Donor site
closed primarily. Patient was
kept on heparin to prevent thrombosis at anastomosis site. Post
operative recovery was uneventful. Patient was discharged on 10th post
operative day. Patient was followed for 3 month. Postoperatively patient
was kept on pentaxyphyllin and tocopherol.
Discussion
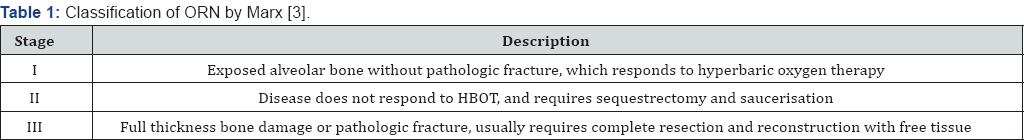
Osteoradionecrosis of facial bone is the rare
complication of radiotherapy given for head neck cancer. Mandible is
most commonly involved bone in osteoradionecrosis (Table 1).
Pathophysiology for osteoradionecrosis is radiation induced hypoxic
injury at cellular level. Hypoxic injury leads to tissue break down
resulted in chronic non healing ulcer. Obliteration of capillaries and
larger vessels along with radiation fibrosis in ischemia of the tissues [5].
Osteoradionecrosis is a possible complication following radiotherapy
where an area of bone does not heal from irradiation of bones causes'
damage to osteocytes and impairs the blood supply. Incidence
osteoradionecrosis is 3.0% in recent studies [6].
Bone injury can occur through.
I. Spontaneous (37%)
II. Direct trauma (63%)
a. Tooth extraction
b. related cancer surgery or biopsy
c. By exposure of oral cavity to the environment
The clinical risk factors of ORN can be divided into
local and systemic. Some of the local factors include tumor stage, tumor
site, dose or radiation (>50-60 Gy), radiation field, dental
extraction and poor oral hygiene, whereas systemic factors include
infection, immune deficient states, co-morbidities and malnutrition [7]. Use of IMRT has reduced the incident of osteoradionecrosis in most of studies [8] (Figures 1-3).


Conclusion
Early stage ORN is approached conservatively with
local wound care, HBO therapy and antibiotic therapy. Stage III patients
are treated with aggressive surgical extirpation of all diseased hard
and soft tissue, and then immediate reconstruction is performed using
free tissue transfer [9]. Free osteocutaneous fibula flap is best reconstructive option to for segmental mandibular body defect.
To read more articles in Journal of
Orthopedic & Orthoplastic Surgery
To
Know More about Juniper Publishers click
on: https://juniperpublishers.com/ 



Comments
Post a Comment